| Back to Back Issues Page |
 |
|
Newsletter - New Secrets About Health and Wellness - Lowering Cholesterols, Homocysteine and Triglyc December 21, 2013 |
Yours in Health and WellnessLowering YOUR Cholesterol, Triglycerides and HomocysteineThe Take-Aways1. Homocysteine can easily be brought to a healthy level in over 90% of cases. 2. Triglycerides can easily be brought to a healthy level in most cases. 3. CoQ10 is essential to many functions including energy production and is concentrated in key organs including the heart. Age, and cholesterol –lowering drugs (CLDs) like statins, significantly lower your body’s CoQ10 levels. 4. Lifestyle, Education, Activity and Nutrition can positively impact cholesterol levels without the negative side-effects of CLDs. 5. If you are on CLDs, consult your physician before stopping your meds. But seriously consult – present the evidence from the previous newsletters and from this one, and discuss a feasible plan for you. 6. If you have moderately elevated cholesterol, and are not on CLDs, use this evidence to have a serious discussion and develop a plan with your doctor before taking statins. HomocysteineIf you have not read the Newsletter in which I discussed the role of homocysteine as an independent factor in Cardio-Vascular Disease, heart disease, and Alzheimer’s you can review it here (new window).Bringing your homocysteine to a safe level is easily achieved by most people. In 1995 Boushey et al reported in the Journal of the American Medical Association that about 27 mg/day of B6, 60 mcg/day of B12 and 1000 mcg/day of folic acid will lower homocysteine levels to safe, normal levels. (1) The same year it was reported that if we take 1000 mcg of folic acid along with Vitamins B6and B12 in supplementation each day, 92% of homocysteine levels would fall to a safe range. (2) In 1999 Loba and associates studied a combination of low-dose folic acid combined with Vitamins B6 and B12 to reduce homocysteine levels in patients with cardio-vascular disease. Patients received 400 mcg, 1 mg or 5 mg of folic acid, 12.5 mg of B6 and 500 mcg of B12. They concluded that a daily dose of 400 mcg of folic acid combined with the B vitamins normalized homocysteine levels in patients with cardio-vascular disease. (3) In 2000 there was an interesting randomized, placebo-controlled trial among 158 healthy siblings of 167 patients with premature atherothrombotic disease (“hardening of the arteries”). In the study, 80 of the healthy siblings were assigned placebo and 78 were assigned 5 mg folic acid with 250 mg Vitamin B6 daily for 2 years. There was a significant decrease in homocysteine levels in those using B6 and folic acid and they had a decreased rate of abnormal exercise electrocardiography tests – which is consistent with a decreased risk of atherosclerotic coronary events. (4)
So for most people elevated levels of homocysteine can easily be brought to a healthy level.
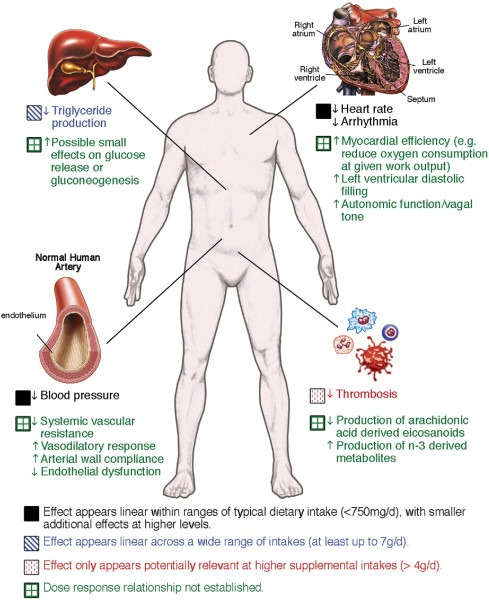
TriglyceridesIn brief, supplementation with purified fish oil, from which contaminants have been removed, lowers triglycerides significantly; in my case by 63%. Fish oils typically contain the two essential Omega 3 fatty acids: Docosahexaenoic acid (DHA) and Eicosapentaenoic acid (EPA).In 2007 Darshan S Kelley et al reported in the American Journal of Clinical Nutrition that supplementation with DHA (either 7.5 g DHA oil/d and then 3 g DHA/d) or olive oil (placebo) for the last 90 d) “may improve cardiovascular health by lowering concentrations of triacylglycerols and small, dense LDL particles”. (5) In 2011 a study by Ann C Skulas-Ray et al reported in the American Journal of Clinical Nutrition found that Omega 3 (DHA + EPA) at 3.4 g/day lowered triglycerides by 27% compared with placebo. This was a placebo-controlled, double-blind, randomized, 3-period crossover trial (8 weeks of treatment, 6 weeks of washout) that compared the effects of 0.85 and 3.4 g EPA+DHA/d in 23 men and 3 postmenopausal women with moderate hypertriglyceridemia (150–500 mg/dL). (6) In the same year Mozaffarian and Wu noted in a meta-analysis that the effectiveness of Omega 3 in “lowering of plasma triglycerides is well recognized”. They recommend that “if significant triglyceride-lowering is a goal, then concentrated over-the-counter or prescription formulations are preferable to facilitate sufficiently high doses (>3 g/day EPA+DHA) with reasonable daily numbers of capsules”. They also note that “concerns have been raised over potential harm from contaminants present in some fish species, such as methylmercury, dioxins, and polychlorinated biphenyls (PCBs)”. (7) So if you buy Omega 3 oil you need to be certain that all contaminants have been removed by a double molecular distillation process. Double molecular distillation improves quality and stability – removes heavy metals including mercury, pesticides, PCBs, and organic residues. At least one company , and definitely not all, guarantees the purity and potency of its Omega 3. This graphic from the Mozaffarian and Wu meta-analysis (7) outlines the range of benefits associated with Omega 3 and Cardio-Vascular Disease.
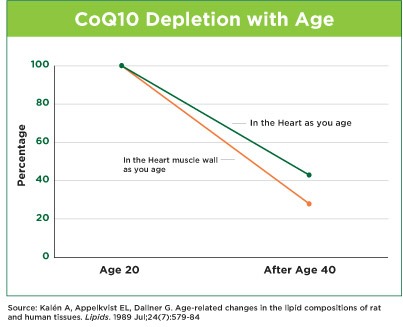
Omega 3s will bring triglycerides to a healthy level in most cases, as well as providing numerous additional health benefits. CoEnzymeQ10ATP, or adenosine-5-triphosphate, is a molecule in which our cells store energy. ATP is synthesized and used by the mitochondria of every cell in your body. Isn’t that amazing? In every one of the trillions of cells in your body. CoQ10 is important because it an absolutely essential part of the electron transport chain that produces ATP. No CoQ10 …. No ATP.Our ability to metabolize CoQ10 from food sources decreases quite dramatically with age as seen in the following graph. So as we age we make less of this critical element that is concentrated in your heart and other critical organs like the liver, kidney and pancreas. In 1989 Anders Kalen et al reported in Lipids that in human pancreas and adrenal the CoQ10 content was highest at one year of age, whereas in other organs the corresponding peak value was at 20 years of age, and was followed by a continuous decrease upon further aging. This is illustrated in the following graph. (8)
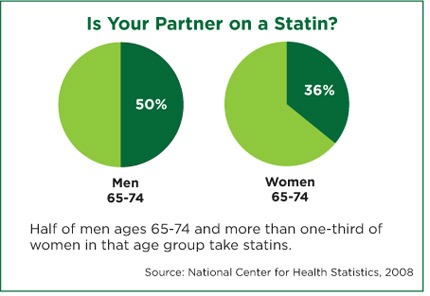
Marcia Wyman, PharmD. in her 2010 review article cited below (11) referenced 7 studies reported in peer-reviewed journals showing how statins reduced CoQ10 while reducing cholesterol. Given the critical role played by CoQ10 and the fact that our body produces less and less as we age, in the period of life when most statins would be prescribed, this is shocking and important. We need to pay attention to this. The following chart shows the high use of statins in treating elevated cholesterol.
Supplementation with CoQ10 has been shown to be an effective treatment for people with isolated systolic hypertension (ISH) - higher blood pressure number (systolic) is elevated. When patients were supplemented with 120 mg/day CoQ10 or placebo for 12 weeks, those on CoQ10 experienced and average 18 mm Hg reduction in systolic dropping from 165 to 147 mm Hg while the placebo group experienced a negligible reduction of 2 mm Hg. At least 5 clinical trials had similar results. (9) An earlier double blind, placebo controlled study had similar outcomes when 60 mg of CoQ10 were administered twice daily for 8 weeks to 30 patients and a B vitamin complex was administered to 29 patients: all patients were known to have essential hypertension and were presenting with coronary artery disease (CAD). All patients were already receiving antihypertensive drugs. In the CoQ Other studies replicating these results can be found in a 2010 review article by Marcia Wyman, PharmD. (11) Improving the HDL Ratio of Total CholesterolYou will recall from the Newsletter on Cholesterol (new window) that High Density Lipoprotein (HDL) is the good cholesterol. As noted in that issue of my newsletter, at the 2004 American Heart Association Annual Scientific Sessions presenters from Tufts – New England Medical Centre, reported on a meta-analysis of 17 major lipid lowering trials involving 44,170 patients and involving 3,869 fatal or non-fatal heart attacks. They found that the increase in HDL was the best predictor of decreased risk of heart attack, and clearly a better predictor than lowering LDL. Their analysis also showed that there was no marked reduction in risk of heart attack until LDL was reduced by more than 30%. (12) A 1994 study in the Journal of Hypertension reported on 350 men and women with slight hypertension who were given 6 grams of purified fish oil, or a placebo, once per day for 6 months. While hypertension was not affected, the levels of HDL (the good cholesterol) were significantly increased, especially in the women. (13)Lowering Your LDLAs already outlined above, supplementation with DHA (from Omega 3) decreases the concentration of small, dense LDL particles. (5)Transfats raise LDL and decrease HDL. That is, of course, not the way you want to go. Transfats are heavily used in processed foods in the form of vegetable oils (corn, soy, or safflower). Previous newsletters on GMOs explain that a very, very high proportion of corn and soy crops are GMO, another reason to avoid them.
Monounsaturated fats include olive oil (always buy Extra Virgin in a dark bottle to prevent degradation), canola oil (which I don’t recommend because so much canola is genetically modified); nuts, seeds, avocados, and olives. Polyunsatured fats are found in nuts (almonds and walnuts are very good), seeds (chia, flax, quinoa, pumpkin and squash) and oils from sunflowers. When you cook with olive oil remember “in order to preserve virgin olive oil bioactive components heating time should be reduced to the minimum”. Think about the fact that “as most of its bioactive components, including phenolic compounds, are gradually lost, it is economically advantageous to use lower olive oil grades and frequent replenishment under prolonged thermal processing” i.e. cooking. (14) Another alternative is to use coconut oil in cooking, especially frying.
The effects of mono-unsaturated fats were assessed in a 2004 study. In a parallel-arm design study, 53 overweight and obese healthy men and women were randomly assigned to a low fat (18% of energy intake) or moderate (33% of energy intake) diet for 6 weeks to achieve weight loss followed by 4 weeks of weight maintenance. For the moderate fat diet monounsaturated fats (MUFA) were used – 50% of the fat consumed in this group was from peanuts, peanut butter and peanut oil – all MUFAs. In the moderate fat diet group HDL (good) cholesterol was unchanged and triacylglycerol and ratios of total and non-HDL to HDL cholesterol were all improved. In other words LDL dropped in the moderate fat diet group while HDL remained constant. The low fat diet did not achieve positive changes in cholesterol; in fact they decreased HDL by 12%, not a good outcome. (15)
In a large scale study a detailed medical and lifestyle history, including diet, was obtained through an interview. 4466 adult participants of the National Heart, Lung, and Blood Institute (NHLBI) Family Heart Study were involved. “The wide age range, the availability of data across many centers, and the large sample size are strengths of the study.”
The data showed that the consumption of fruit and vegetables is associated with lower concentrations of LDL cholesterol in a dose-response manner. The more fruit and vegetables, the lower the LDL. (16) In a 2006 review article in the Journal of Lipid Research Lichtenstein noted that in previous studies “the total cholesterol-to-HDL cholesterol ratio is similar and more favorable for polyunsaturated and monounsaturated fatty acids than for saturated fatty acids. Similarly, observational data suggest polyunsaturated and monounsaturated fatty acid, relative to saturated fatty acids, intakes are associated with reduced CVD risk”. (17) LEANLEAN, is that not a great acronym? Easy to remember and a useful reminder.
So what’s it mean? Lifestyle Education Activity Nutrition
Let’s examine some key elements of each as they relate to healthy cholesterol levels. Lifestyle will be covered in the next Newsletter because it is too large to cover here.
Education means informing yourself with evidence–based information. Watch out, because the Internet, magazines, TV, radio talk shows, newspapers, web blogs and many books are filled with superficial and/or incorrect information. The old maxim Caveat Emptor – Buyer Beware definitely applies in the Information Age. Sure you can find information on any topic at the click of a mouse. But you really need to be sure that it is accurate and valid – that it is evidence-based. That is why I make every effort to provide you with the findings of scientific medical research found in peer-reviewed medical journals.
Activity can assist in lowering lipid levels. Exercise is known to improve lipoprotein levels, whereas an elevated body mass index (BMI) is associated with less favorable lipoprotein levels. This study by Garry and McShane evaluated the lipid-lipoprotein profiles in a group of 70 professional football players from one NFL team to determine the association between these profiles and the players’ BMIs. Measurements included BMI (kg.m-2 ), and fasting serum lipid analysis. Linemen have the highest mean BMI, 38.1 kg.m-2 . Comparing mean lipid values among BMI categories demonstrated lower HDL, higher triglycerides (p<0.005) higher total cholesterol/HDL ratios with an increasing BMI. They concluded that among the elite athletes in this study with the highest BMIs, exercise may not confer the same protective benefits on cardiovascular risk as it does in those athletes with normal BMIs. (18)
Both uphill and downhill exercise were shown in a small (45 people) randomized, crossover study to be heart healthy with some differences between the two forms of exercise (concentric and eccentric respectively). The sedentary, non-diabetic subjects were randomized to 2 months of hiking up mountains (gondola down) or to hiking down mountains (gondola up) at least 3-5 times per week. After 2 months the tasks were reversed for each group. Triglycerides were lowered only by concentric exercise (uphill) and glucose tolerance was most improved by eccentric exercise (downhill). Uphill exercise reduced LDL cholesterol by 10.2% and downhill by 8.9%. Other forms of concentric and eccentric exercise should produce similar results. (19) So hike up and hike down. Steep hills would be an option. Come live in White Rock, North Vancouver or San Francisco and walk everywhere. Physical activity throughout life reduces the risks for cardiovascular disease. A study by Sandrock et al in the 2008 British Journal of Sports Medicine compared a number of indicators between two groups of men. One group of 51 men (mean age 64.48 years) had been physically active throughout life; the second group of 50 men (mean age 64.37 years) had not been physically active. All the men in both groups were “healthy”. There was a significant difference between the two groups (in favour of the active group) on a number of measures – LDL cholesterol and triglyceride levels, roughness of intima-media, atherosclerosis in the common carotid artery. (20) A meta- analysis in the same journal covering 459,833 participants (male and female) who were free from CVD at the outset, were followed for walking patterns. A total of 19,249 had died by follow-up. The analysis showed that those in the highest walking category had 0.69 the risk of those in the lowest walking category. The best results were more highly linked to those who walked faster than to those who walked the most. (21) A 2008 study at McMaster University involved 28 older men and women (mean age 68.5 +/- 5.1 years) in whole body resistance training for 14 weeks. Prior to and 72 hours after the last exercise routine biopsies were taken from the largest part of the thigh quadriceps muscle. Urine samples were also taken. No changes were noted in the mitochondrial DNA. An increase in complex IV of the electron transport chain (see CoQ10 above) suggests increased antioxidant effect as a result of this exercise regimen. (22) These studies and others illustrate the importance of exercise throughout the life span, from childhood to the 90’s. So wherever you are it’s not too soon to start and it’s not too late. But the sooner you start the greater the benefit throughout your lifespan.
Nutrition, you might have noticed, is a big part of what is already covered in this Newsletter. Your food selections have a lot to do with cholesterol (HDL, LDL and other forms), homocysteine and triglycerides.
Think of the old ditty about computers: GIGO – Garbage In Garbage Out. While that’s true of computers it’s also true of our bodies, except that the Garbage Out part refers to the garbage that after processing by our digestive system, goes to our cells. If you’re sleepy after eating it’s likely that you are practising Garbage In, or you are simply consuming too much food.
A good rule of thumb, in food choice, is to shop around the perimeter of your supermarket where the whole foods, including fruits and vegetables are usually found. Stay away from the rows of aisles in the center where the processed and junk foods are found.
The Take-AwaysLet’s save space. Scroll back to the top for the important takeaways.Yours in health and wellness. Roger BTW Want to support
moms fighting against GMOs? (new window)
Footnotes1. JAMA 1995; 1049-572. Lancet 1995; (345):85-89 3. Am J Cardiol 1999; 83:821-5 4. Lancet 2000; 355(9203):517-22 5. Am J Clin Nutr 2007;86:324 –33 6. Am J Clin Nutr 2011:93 (2) 243-252 7. J Am Coll Cardiol 2011;58(20):2047-2067 8. Lipids 1989 24(7):579-84 9. South Med J 2001; 94: 1112-1117 10. J Hum Hypertens 1999 Mar;13(3):203-8 11. Cleveland Clinic Journal of Medicine July 2010 vol. 77 7 435-442 12. Circulation 2004; 110: 227-239 13. J Hypertens Suppl. 1994;12(7):S23-31 14. Food Research International 2013 (54):2016–2024 15. Am J Clin Nutr 2004;79:204-212 16. Am J Clin Nutr 2004:213-217 17. The Journal of Lipid Research, 2006; (47):1661-1667 18. Prev cardiol 2001; Summer 4(3): 103-108 19. AHA 2004 Scientific Sessions :Abstract 3826 (Nov 10) 20. Br J Sports Med 2008; 42:839-844 21. Br J Sports Med 2008; 42:238-243 22. Exper Gerentol 2005; 40(3):173-180 |
| Back to Back Issues Page |